Measuring the Silent Fracture Copy
3.1.3 Measuring the Silent Fracture
t bears repeating some of the facts and statistics reviewed in Module 1, with respect to vertebral fractures in particular:
- A 50-year-old woman has a 40% chance of developing hip, vertebral or wrist fractures during her lifetime.36
- Patients are at highest risk for subsequent fracture in the first few months following a vertebral fracture.26
- 1 in 4 women who have a new vertebral fracture will fracture again within one year.31
- Both vertebral and hip fractures are associated with an increased risk of death.
It has also been noted that more than 60% of vertebral fractures are ‘silent’ in nature, that is not accompanied by any overt pain or immediate structural changes20. Even more striking is that while these are by far the most common type of fracture in osteoporotic population, the majority (66%) do not gain clinical attention.47
There are four easy, clinical measures that can help identify these silent fractures.
1. Historical Height Loss (HHL)
As the name suggests, this refers to the amount of height that an individual has lost over his or her lifetime. Simply calculate the difference between a person’s tallest height recalled against their current measured height.
Ensure accurate current height measures by:
- using wall-mounted devices if possible
- careful positioning of patient each time (where the inferior border of the bony orbit is in line with the groove at the top of the tragus of the ear)
- repeat measures 3 times (repositioning each time) and average to the closest millimetre
Practice guidelines suggest that individuals over age 60 with >6cm HHL and individuals under age 60 with >4cm HHL be referred for spine radiographs as this is indicative of present vertebral fractures.
2. Prospective Height Loss (PHL)
For patients being followed over time by a clinician, changes in height between subsequent visits can be monitored (up to a 3-year time frame).
Presence of vertebral fractures is indicated with a loss of >2cm PHL measure.
3. Wall-Occiput Distance (WOD)
This measure is useful in the presence of frank or developing kyphosis. Since postural compensatory changes may be present, it is important to reveal the upper back, and position the patient against the wall such that:
- back and heels are against the wall
- facing straight ahead
- a measurement of the distance between the wall and occipital prominence is made
WOD greater than 5 cm is indicative of a vertebral fracture likely present in the thoracic spine.
4. Rib-Pelvic Distance (RPD)
Vertebral fractures in the lumbar spine can also cause postural changes and compensations. The distance between the ribs and pelvis (iliocostal distance) can be measure to assess this postural change. In order to measure this:
- stand behind patient (who is also standing)
- palpate the bottom ribs and iliac crest in the mid-axillary line
- determine the vertical distance between the rib and iliac crest by either fingerbreadths or measurement of skin markings.
An RPD of less than 2 fingerbreadths or 3.6cm suggests the presence of a vertebral fracture, likely in the lumbar region.
Adapted from two articles by Kerry Siminoski MD published in the Spring & Winter 2005 issues of Osteoporosis Update.47
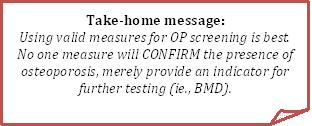
Bottom Line Caution:
No single physical exam finding can rule in osteoporosis or fracture without further testing. The above measures are easy clinical tests which would identify patients who may benefit from early screening/BMD testing.
Assessment Tools:
Osteoporosis Canada has provided guidelines for BMD testing (outlined in detail in Module 1). In brief, the following can be applied:
- Everyone 65+ is recommended to have a BMD test
- Patients over the age of 50, with risk factors for fracture, should have BMD testing
- Clinically determine management decisions using the 10-year absolute fracture risk assessment tools CAROC and/or FRAX
In addition, the following two tools have been identified in current research9 to be sensitive and valid in assisting the clinician to make decisions regarding BMD testing.
1. Osteoporosis Risk Assessment Instrument (ORAI)
Calculation of score – points given for:
- age: 15pts if 75+; 9 pts if 65-74; 5 pts if 55-65
- weight: 9pts if <60kg; 3 if 60-69.9kg
- 2pts if not currently taking estrogen
Interpretation of score:
- recommend BMD if ORAI >8
- low risk: <9; medium risk: 9-17; high risk: >17
(Cadarette, 2000; Development and validation of ORAI)
2. Osteoporosis Self-Assessment Tool (OST)
Calculation of score:
- 0.2x(weight in kg-age in years)
- truncate to yield integer
Interpretation of score:
- recommend BMD if OST<2
- low risk: >1; medium risk: -3 to 1; high risk: <-3
(Koh, 2001; A simple tool to identify Asian women at risk of OP)