The Guidelines are scheduled to be updated late 2020 or early 2021.
Management Guidelines Copy
Introduction to this section
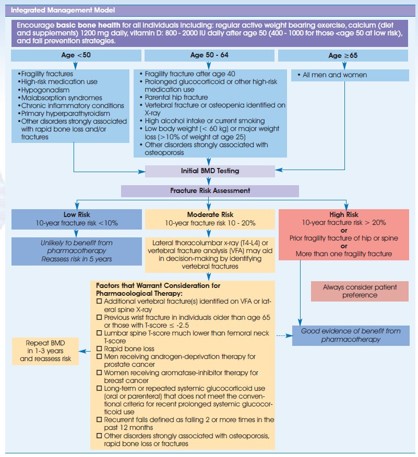
Once a client’s fracture risk is determined, from a medical management perspective there are several interventions that would be recommended or prescribed by the medical team. These include nutrition & supplementation, exercise, lifestyle modifications and prescription medicines. In this workshop, we will focus on exercise and adapting activities mainly but for completeness, below is more information on the other interventions.
Integrated Management Model
Learn more about the Clinical Practice Guidelines (2010)
Bisphosphonates
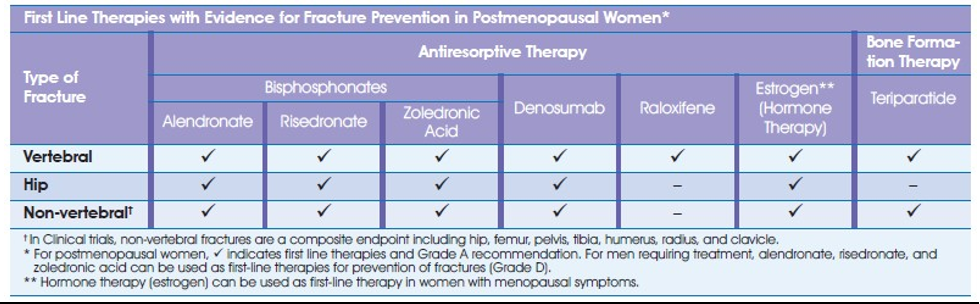
Bisphosphonates are a family of drugs used to treat osteoporosis. There are four bisphosphonates currently approved for use in Canada: alendronate (Fosamax ®), etidronate (Didrocal ®), risedronate (Actonel ®) and zoledronic acid (Aclasta®). Also available are: Actonel® Plus Calcium and Fosavance® (Fosamax® with vitamin D).
How do they work?
Bisphosphonates bind to the surfaces of the bones and slow down the bone resorbing action of the osteoclasts. This allows the osteoblasts to work more effectively.
How effective are they?
All four bisphosphonates increase bone density and prevent vertebral fractures. Alendronate, risedronate and zoledronic acid have also been shown to prevent hip and non-vertebral fractures.
Who can take them?
Bisphosphonates are used to treat osteoporosis in: postmenopausal women and in men; and in men and women of any age who are using steroid medications.
How are they taken?
Bisphosphonates have very specific instructions about how they must be taken in order to be absorbed properly and avoid side effects. Because calcium interferes with the absorption of bisphosphonates, calcium supplements must be taken at other times of the day. See details on Osteoporosis Canada website.
Are there side effects?
The most common side effects are nausea, abdominal pain and loose bowel movements. Bone, joint and/or muscle pain has been infrequently reported in patients taking bisphosphonates. There is a small risk of ulcers in the esophagus with both alendronate and risedronate, especially if taken incorrectly.
The most common side effects of zoledronic acid, which usually only last a day or two, are fever, pain in the muscles, bones or joints and headache. There have been rare cases of acute renal dysfunction following infusion of zoledronic acid.
In very rare cases, alendronate, risedronate and zoledronic acid have been linked to a breakdown of the jaw bone (called osteonecrosis of the jaw) following dental work such as dental extractions. Rare cases of atypical fractures of the femoral (thigh) bone have been reported with bisphosphonates. One should notify their physician if they experience pain in the groin or thigh that is present for a few weeks.
Denosumab
Denosumab (Prolia®) belongs to a class of osteoporosis treatment called a Rank ligand inhibitor.
How Does Denosumab Work?
Denosumab is an anti-resorptive treatment that inhibits the development and activation of osteoclasts (the cells that eat away bone).
How Effective Is It?
Denosumab reduces the risk of fractures of the spine, hip and other sites in women with postmenopausal osteoporosis.
Who Can Take It?
Denosumab can be used to reduce the risk of fractures in postmenopausal women with osteoporosis.
As of October 2010, the clinical trials using denosumab in men with osteoporosis are ongoing.
How Is It Taken?
Denosumab is an injection under the skin given by a trained healthcare professional, twice a year.
The dose is 60 mg.
Are There Side Effects?
Side effects may include pain in the muscles, arms, legs or back and a skin condition with itching,
redness and/or dryness. It also slightly increases the risk of cellulitis, a skin infection that is treated with antibiotics. In rare cases, osteonecrosis of the jaw has been reported in patients treated with Denosumab.
Parathyroid Hormone
Parathyroid hormone (PTH) and its analogue, teriparatide, are a class of osteoporosis treatments called bone formation agents. Teriparatide injection (Forteo) is the first medication approved by Health Canada in this new class.
How does teriparatide injection work?
The mechanism by which bone is constantly renewed is called bone remodelling. Teriparatide injection works in a novel way on the bone remodelling process so that new bone is generated and added to the skeleton faster than old bone is broken down. It does this by activating the osteoblast (bone-building) cells.
How effective is it?
Teriparatide injection has been shown to increase bone density and reduce the risk of both vertebral fractures and other fractures associated with osteoporosis.
Who can take it?
It is used for the treatment of postmenopausal women with severe osteoporosis who are at high risk of fracture or who have failed or are intolerant to previous osteoporosis therapy. It is also used to increase bone mass in men with primary or hypogonadal (low testosterone) severe osteoporosis who have failed or are intolerant to previous osteoporosis therapy. It is also indicated for the treatment of osteoporosis associated with sustained systemic glucocorticoid therapy in men and women who are at increased risk of fracture.
How is it taken?
It is taken as a sub-cutaneous injection into the thigh or abdominal wall, 20 mcg (micrograms) once a day. This medication should not be taken for longer than 24 months.
Are there side effects?
Possible side effects include dizziness, nausea and leg cramps.
Supplements
Calcium: An essential element for life
Calcium is crucial to maintain life. Just about every cell in the body, including those in the heart, nerves and muscles, relies on calcium to function properly and bones require calcium to maintain their strength. The main goal of good calcium nutrition is to maintain an adequate supply so that our bodies do not have to dip into our only calcium reservoir - our bones.
Vitamin D: A key factor in good calcium absorption
The body makes vitamin D when exposed to sunlight. Since most Canadians don't always get enough sun exposure and it may be difficult to obtain necessary amounts of vitamin D through diet alone, supplements are generally a good idea. Vitamin D3 increases calcium absorption by as much as 30 percent. Osteoporosis Canada recommends that Canadians aged 19 to 50, including pregnant or lactating women, receive 400 - 1000 international units (IU) of vitamin D3 per day. Adults over 50 should receive 800-2000IU
In the body, calcium is found in three places: in the skeleton and teeth, in the cells, in the blood. Because calcium is so important, the body has a carefully regulated system to ensure that a good supply is always - and immediately - available. The body does this in three ways:
- It absorbs calcium directly from the food we eat.
- It takes calcium from our bones if there is not enough available. When this happens, the bones become less dense and more fragile.
- It slows down the amount of calcium that leaves the body in the urine by returning some to the blood
- stream where it remains available to organs and cells.
The role of calcium in building stronger bones
- By age 20 in men and age 16 in women, bones typically stop growing in length and we are almost at our peak bone mass – calcium plays a large role in achieving that peak bone mass.
How to maximize calcium intake through diet
Getting an adequate amount of calcium every day
Consult a reliable food chart (see the Osteoporosis Website for sample food chart and calcium calculator) which shows the calcium content of specific foods and compare against chart above to determine if an adequate amount is being obtained through diet alone.
Eat foods that contain calcium that is easily absorbed.
Dairy products such as milk, cheese and yogurt are excellent sources of calcium because they contain high amounts of calcium that are easily absorbed by the body. Skim milk products provide as much calcium as whole milk with the added advantage of less fat and cholesterol. Some calcium-fortified soy beverages and orange juices may contain as much calcium as milk (check the labels). Vegetables also provide calcium, as do fish products containing bones (canned salmon and sardines) and meat alternatives such as lentils and beans.
Calcium Supplements
Calcium supplements are tablets, capsules or liquids containing the mineral calcium from a non-food source.
These sources include:
Calcium carbonate, which can be refined from limestone, natural elements of the earth, or may come from shell sources, usually oyster. Shell sources are often described on the label as a "natural" source. Calcium carbonate from oyster shells is not "refined" and can contain variable amounts of lead.
Chelated calcium, which refers to a special way in which calcium is chemically combined with another substance. Calcium citrate is an example of such a chelated preparation. Calcium may also be combined with other substances to form preparations such as calcium lactate or calcium gluconate.
Powdered bone (bonemeal) or dolomite, a mineral found in rock. (Bonemeal is not recommended, as it may contain contaminants.)
Physical Activity and Exercise
Physical activity is an important factor in the risk reduction and treatment of osteoporosis. Physical activity places an increased "load" or force on our bones. Bones respond by forming new bone and remodelling the bone to be stronger. Bones need to be stimulated by physical activity -- so it is necessary to be active in different ways in order to "load" or stimulate these bones and maintain their structural competence and strength.
Physical activity also contributes to a sense of well-being and an overall improvement in quality of life as well as improving balance and coordination which, in turn, reduces risk of falling -- falls that can result in fractures. In addition, improved strength, flexibility and posture can reduce pain and enable people with osteoporosis to do daily tasks more easily.
There are 4 types of exercise and activity integral to the management of low trauma fracture and osteoporosis:
- Strength
- Posture and core stability
- Balance
- Weight-bearing
Exercise will be discussed in much more detail later in this workshop.

Optimal Strain for Maintaining and Building Bone
Good News
Bad News
To maintain bone, low magnitude strains work
Exercise Types
‘Any’ is good (On bedrest, bone loss of about 1% per week and regain at about 1% per month)
High impact (jumping) is best yet studied in children and premenopausal women
Exercise preserves bone mass and maximizes bone geometry in adults
- Weight bearing: meta-analysis showed about a 1% maintenance of bone per year in pre and post-menopausal women
- Progressive resistive/strength training: systematic review and meta-analysis showed about a 1% maintenance of bone